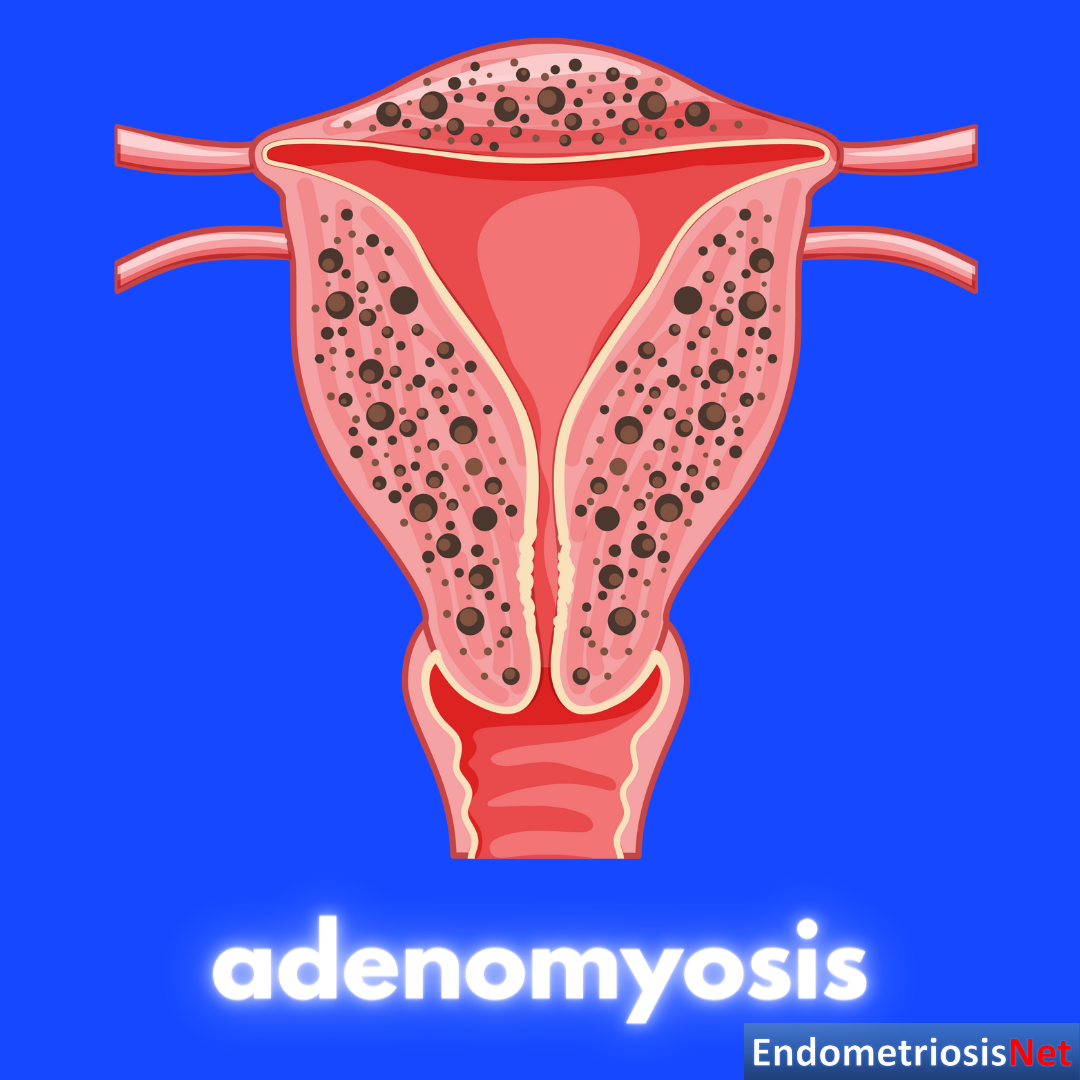
Η αδενομύωση είναι μια κοινή, καλοήθης νόσος της μήτρας, κατά την οποία ο ιστός ο οποίος καλύπτει το εσωτερικό της μήτρας (ενδομήτριο) βρίσκεται μέσα στο μυϊκό τοίχωμα της μήτρας (μυομήτριο). Είναι άγνωστης αιτιολογίας και χαρακτηρίζεται από βαριές κι επώδυνες περιόδους, ενώ σχετίζεται και με υπογονιμότητα.
Πόσο συχνή είναι η αδενομύωση;
Αν κι η ακριβής συχνότητα δεν είναι γνωστή, υπολογίζεται πως προσβάλλει έως και 20% των ασθενών που επισκέπτονται τον γυναικολόγο. Είναι πιο συχνή σε γυναίκες μέσης ηλικίας και σε αυτές που έχουν υποβληθεί σε χειρουργική επέμβαση στη μήτρα ενώ, συχνά, συνυπάρχει με άλλες γυναικολογικές νόσους ευαίσθητες στα οιστρογόνα, όπως η ενδομητρίωση και τα ινομυώματα.
Πώς γίνεται η διάγνωση;
Στο (όχι και τόσο μακρινό) παρελθόν, η διάγνωση της αδενομύωσης ήταν ιστοπαθολογική (απαιτούνταν, δηλαδή, μικροσκοπική ανάλυση της μήτρας που είχε αφαιρεθεί με υστερεκτομή). Με την πρόοδο των μη επεμβατικών, ακτινολογικών μεθόδων, είναι πλέον δυνατή η διάγνωση της αδενομύωσης τόσο με το διακολπικό υπερηχογράφημα όσο και με τη μαγνητική τομογραφία πυέλου, με βάση την παρουσία συγκεκριμένων διαγνωστικών κριτηρίων. Αξίζει, επίσης, να σημειωθεί πως αναγνωρίζονται διαφορετικοί τύποι αδενομύωσης: διάχυτη, εστιακή, κυστική και συμπαγής.
Φαρμακευτική αντιμετώπιση:
Σε αυτές περιλαμβάνονται το κλασσικό αντισυλληπτικό χάπι (οιστρογόνο+ προγεσταγόνο), προγεσταγόνα με διαφορετικές οδούς χορήγησης (δισκία, ενδομήτριο σπείραμα, ενέσιμο, υποδόριο εμφύτευμα) καθώς και αγωνιστές GnRH, π.χ. ενέσεις Arvekap.Μια νέα, πολλά υποσχόμενη επιλογή είναι οι ανταγωνιστές GnRH, οι οποίοι μπορούν να χορηγηθούν από του στόματος. Μιας κι η αδενομύωση είναι, όπως αναφέραμε, μια ορμονο-ευαίσθητη νόσος, η φαρμακευτική της αντιμετώπιση βασίζεται στη χορήγηση ορμονών με κύριο στόχο τη βελτίωση των συμπτωμάτων της μηνορραγίας (‘’βαριά περίοδος’’) και της δυσμηνόρροιας (έντονος πόνος κατά την περίοδο) και την αποφυγή μιας χειρουργικής επέμβασης. Αν και συχνά επιτυχής, δεν είναι αποδεκτή από πολλές ασθενείς λόγω πιθανών παρενεργειών, μη επιθυμίας χρήσης ορμονών κι άμεσης επιθυμίας για εγκυμοσύνη.
Χειρουργικές μέθοδοι:
Σε γυναίκες με έντονα συμπτώματα, οι οποίες έχουν ολοκληρώσει την τεκνοποίηση, η λαπαροσκοπική υστερεκτομή (αφαίρεση της μήτρας με διατήρηση των ωοθηκών) προσφέρει άμεση ανακούφιση από τα συμπτώματα, ειδικά στη διάχυτη αδενομύωση. Ωστόσο, πολλές από τις ασθενείς δεν έχουν ολοκληρώσει την τεκνοποίηση ή δεν επιθυμούν να υποβληθούν σε υστερεκτομή. Αυτό οδήγησε στην εφαρμογή χειρουργικών τεχνικών με διατήρηση της μήτρας (uterus-sparing techniques). Διακρίνονται σε 2 βασικές κατηγορίες: Την αδενομυοματεκτομή (για εστιακή αδενομύωση) και την ‘’κυτταρομειωτική’’ χειρουργική για τη διάχυτη αδενομύωση. Στην πρώτη περίπτωση, αφαιρείται η εστία της αδενομύωσης, χωρίς να αφαιρείται το υγιές τμημα του μυομητρίου, ενώ στη δεύτερη περίπτωση, αναγκαστικά, αφαιρείται σημαντικό τμήμα του μυομητρίου. Στην πρώτη περίπτωση, η επέμβαση μπορεί να γίνει (στα χέρια κατάλληλα εκπαιδευμένων χειρουργών) λαπαροσκοπικά ή υστεροσκοπικά με πολύ ικανοποιητικά αποτελέσματα ενώ στη δεύτερη περίπτωση (όπου η χειρουργική επέμβαση είναι λιγότερο συχνή) απαιτείται, συχνά, λαπαροτομία (ανοικτό χειρουργείο).Σε γυναίκες που έχουν ολοκληρώσει την τεκνοποίηση και δεν επιθυμούν αφαίρεση της μήτρας, μπορούν να εφαρμοστούν διάφορες ελάχιστα επεμβατικές μέθοδοι καυτηριασμού (π.χ. HIFU, radiofrequency ablation κ.ά.).
Αδενομύωση και υπογονιμότητα:
Η νόσος μπορεί να έχει αρνητική επίδραση στην πιθανότητα αυτόματης σύλληψης,st trimester complications, as well as the likelihood of success of various methods of artificial reproductive technology (ART). It, also, appears that the likelihood of pregnancy may further deteriorate as the ‘’severity’’ of adenomyosis (by ultrasound criteria) increases. A link to obstetric complications, such as preterm birth and post-partum haemorrhage appears to exist too. High-quality, surgical excision of adenomyosis may increase chances of conception. Moreover, the pre-treatment use of GnRH agonists before IVF may increase the chances of success.
Συνοπτικά, η αδενομύωση παραμένει μια αινιγματική γυναικολογική νόσος. Αν και ,παλαιότερα, θεωρούνταν νόσος των πολυτόκων γυναικών (αυτών που είχαν γεννήσει περισσότερες από 1 φορές), εμφανίζεται πιο συχνά σε νεότερες γυναίκες και γίνεται πιο ξεκάθαρη η σχέση της με την υπογονιμότητα. Η επιλογή της κατάλληλης μεθόδου αντιμετώπισης πρέπει να εξατομικεύεται, με βάση τα κυρίαρχα συμπτώματα αλλά και τις αναπαραγωγικές επιθυμίες της ασθενούς.