Recurrence of ovarian endometrioma (chocolate cyst) is, unfortunately, not a very rare incident. One may wonder if women with recurrent endometrioma are more likely to also present with deep endometriosis lesions. The answer to this question comes from a recently published study of 611 consecutive women with pelvic pain who underwent surgery for ovarian endometrioma (1). The study found that women operated for recurrent endometriomas have more multiple deep endometriosis lesions and more extensive disease, compared to women with no previous endometrioma surgery.
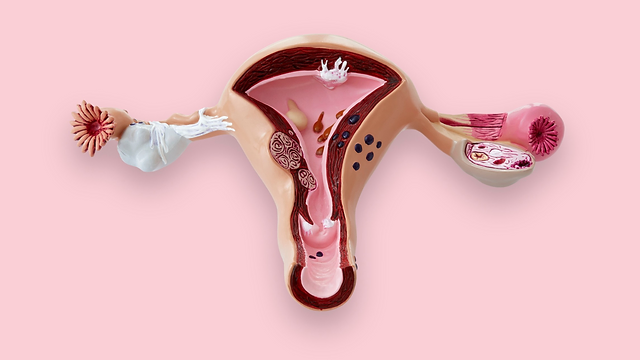
The presence or not of deep endometriosis lesions during a planned endometriosis surgery is crucial information, both for the surgeon and the patient, as it may impact on surgical complexity and recovery. It is true that ovarian endometriomas, particularly in patients with pelvic pain, are seldom isolated, usually co-existing with other endometriosis lesions. However, conditions like bilateral endometriomas or voluminous endometriomas taking up large part of the pelvis may hinder the interpretation of pre-operative imaging, potentially leading to a missed diagnosis of co-existent deep endometriosis lesions, such as bowel endometriosis.
We know that surgery for recurrent endometrioma is technically challenging, even in the absence of co-existent deep endometriosis lesions. Other than the technical aspect itself, repeat ovarian surgery may also have a more profound, negative impact on the ovarian reserve, inducing inadvertent damage to the healthy ovarian cortex (2).
Returning to the aforementioned study of 611 symptomatic women operated for endometrioma (1), patients were divided in 2 groups: The 1st group consisted of 124 patients that had previously undergone excision of endometrioma (via laparoscopy or laparotomy). The 2nd group consisted of 487 patients with no previous surgery for endometrioma. What the authors noted was that women who were operated for recurrent endometrioma were affected by more severe endometriosis, with more multiple deep endometriosis lesions. Longer pain duration and infertility were also associated with presence of deep endometriosis lesions.
Based on this finding, it can be suggested that previous surgery for ovarian endometrioma may be regarded as an independent marker of endometriosis severity. Pelvic pain in patients with endometrioma is closely associated with co-existent deep endometriosis lesions.
But how can we explain the finding of this study (1)? Other studies have suggested that surgery itself may induce endometriosis lesions. In theory, rupture of an endometrioma during previous surgery may seed endometriotic implants.
Complete excision of endometrioma and all associated endometriosis lesions during first surgery may reduce likelihood of recurrence. On the other hand, accurate assessment of risk factors, combined with meticulous imaging as part of the pre-operative work-up may reveal co-existence of deep endometriosis lesions in patients with ovarian endometrioma. This knowledge is important in planning a safe and complete surgical resection of endometriosis.
References:
- Women operated for recurrent endometrioma exhibit more multiple deep infiltrating endometriosis lesions, Parpex et al., JEUD, 2023
- Ferrero S, Scala C, Racca A, Calanni L, Remorgida V, Venturini PL, et al. Second surgery for recurrent unilateral endometriomas and impact on ovarian reserve: a case-control study. Fertil Steril 2015;103:1236–43, doi:http://dx.doi.org/10.1016/j. fertnstert.2015.01.032.